Myanmar’s Health System Faces Crisis Following Earthquake
The recent earthquake in Myanmar has plunged the nation into a severe humanitarian crisis, further straining an already vulnerable healthcare system. As rescue operations are underway and emergency services rush to provide assistance, the limitations of the medical infrastructure are becoming alarmingly clear. Hospitals that previously struggled to cater to their communities now find themselves overwhelmed with a surge of injured individuals and disruptions in essential health services. Public health experts caution that this natural disaster could worsen existing health challenges, leaving millions without vital care. This article explores the precarious condition of Myanmar’s healthcare system and emphasizes the urgent need for international aid to avert a humanitarian catastrophe.
Earthquake Intensifies Healthcare Challenges in Myanmar
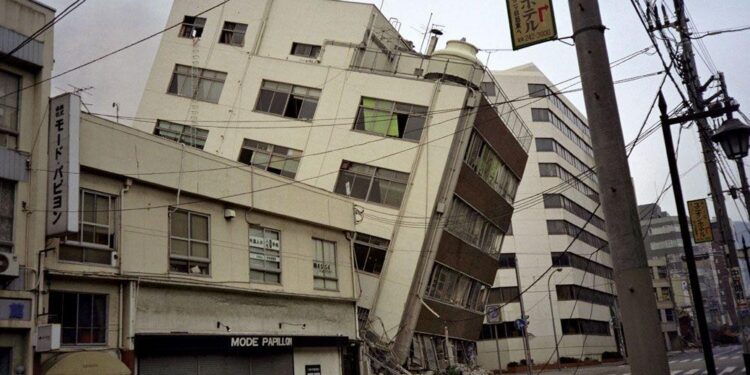
The catastrophic earthquake has deepened Myanmar’s ongoing humanitarian issues, compounding difficulties faced by its beleaguered health system. Displaced populations, overwhelmed medical facilities, and insufficient supplies have created a dire situation that threatens countless lives. The aftermath of this seismic event has exposed significant gaps in healthcare access; many facilities are either damaged or functioning at diminished capacity. The additional influx of trauma cases from the quake is placing unprecedented pressure on a system already strained by conflict and limited public health resources.
Health authorities express concern that combining earthquake-related injuries with persistent diseases such as malaria, tuberculosis, and COVID-19 could lead to disastrous outcomes. Key challenges include:
- Surge in Medical Needs: Hospitals are inundated with patients requiring immediate care.
- Lack of Medical Supplies: Essential medications are running low amid rising demand.
- Interruption of Health Services: Clinics in affected regions have closed or cannot operate effectively.
- Mental Health Concerns: The psychological toll from the earthquake adds another layer to an already heavy burden on public health.
As regional and global aid begins to arrive slowly, addressing urgent healthcare needs remains paramount. However, responses must also tackle underlying systemic issues that have long plagued Myanmar’s healthcare framework. Below is a summary table highlighting critical factors influencing this ongoing crisis:
| Crisis Factor | Description |
|---|---|
| Ongoing Conflict | Diminished availability of health services and resources |
| Poor Infrastructure Quality | Lack of access to medical care for remote communities |
| Disease Outbreak Risks | A higher likelihood of outbreaks due to overcrowded shelters post-disaster |
Emergency Response Limited by Systemic Issues
The recent seismic event has intensified disruptions within Myanmar’s fragile healthcare framework—essential services relied upon by millions are severely impacted. While emergency responders prioritize life-saving measures, critical medical facilities struggle under increased patient loads without adequate treatment options available for many individuals needing care regularly.
- Supply Chain Disruptions: Delays hinder timely delivery of medications necessary for routine treatments.
- Burgeoning Patient Numbers: Hospitals operating at full capacity now face an influx not only from trauma but also chronic conditions left untreated during emergencies.
- Dwindling Resources Allocation: Limited supplies being redirected towards emergency response adversely affect preventive care initiatives across various regions.
This situation reflects not just physical damage but highlights broader systemic failures within public health management as some areas remain inaccessible due blocked routes exacerbated by aftershocks following initial tremors; thus jeopardizing continuity efforts aimed at maintaining essential public health programs amidst political instability complicating coordinated relief actions further still.
The long-term consequences may lead back toward previously controlled diseases such as:
| Disease Type | Potential Consequences |
|---|---|
| Tuberculosis | A rise in transmission rates due lack screening efforts |
| Malaria | An increase if preventive measures aren’t implemented promptly |
| Maternal & Child Health Issues | A spike mortality rates resulting disruption prenatal service provision |
Strategies To Strengthen Myanmar’s Healthcare System Post-Earthquake
As recovery efforts unfold following this devastating quake it becomes increasingly clear there exists an urgent need reformulate strategies aimed bolstering resilience throughout entire national framework surrounding delivery quality accessible affordable comprehensive primary secondary tertiary levels across both urban rural settings alike .
Key initiatives should include :
- Infrastructure Development : Invest building retrofitting hospitals withstand future disasters .
- Training Enhancement Programs : Equip personnel emergency response mental wellness support capabilities .
- Supply Chain Expansion : Establish secure channels ensure consistent flow essential medicines equipment especially remote locations .
Furthermore , fostering partnerships between private sector entities governmental organizations can create sustainable frameworks facilitating ongoing improvements overall quality delivered through collaboration knowledge transfer resource allocation ensuring robust support systems capable responding crises effectively over time.
Timeframe
Action Items
0-6 Months
< tr />
< td >6-12 Months
< td Begin infrastructure enhancements initiate extensive training programs personnel
< tr />
< td >1-3 Years
< td Conduct comprehensive reviews integrate feedback adjust policies accordingly
>
In conclusion , as Myanmar navigates through repercussions stemming from recent earthquakes strains placed upon its fragile systems become increasingly apparent ; limited resources compounded dual challenges treating injuries while maintaining regularity chronic conditions creates uncertainty regarding future prospects available local populations seeking necessary interventions needed maintain healthy lives amidst adversity faced daily . With logistical hurdles hindering international assistance coupled political complexities surrounding governance structures present formidable obstacles ahead yet imperative urgency strategic support never clearer than now ! Resilience exhibited among local workers communities tested weeks reminding us all profound impacts natural disasters exert upon global public-health infrastructures everywhere around world today! Â
Denial of responsibility! asia-news.biz is an automatic aggregator around the
global media. All the content are available free on Internet. We have just
arranged it in one platform for educational purpose only. In each content,
the hyperlink to the primary source is specified. All trademarks belong to
their rightful owners, all materials to their authors. If you are the owner
of the content and do not want us to publish your materials on our website,
please contact us by email – [email protected].. The content will be deleted within 24 hours.ADVERTISEMENT
As recovery efforts unfold following this devastating quake it becomes increasingly clear there exists an urgent need reformulate strategies aimed bolstering resilience throughout entire national framework surrounding delivery quality accessible affordable comprehensive primary secondary tertiary levels across both urban rural settings alike .
Key initiatives should include :
- Infrastructure Development : Invest building retrofitting hospitals withstand future disasters .
- Training Enhancement Programs : Equip personnel emergency response mental wellness support capabilities .
- Supply Chain Expansion : Establish secure channels ensure consistent flow essential medicines equipment especially remote locations .
Furthermore , fostering partnerships between private sector entities governmental organizations can create sustainable frameworks facilitating ongoing improvements overall quality delivered through collaboration knowledge transfer resource allocation ensuring robust support systems capable responding crises effectively over time.
Timeframe
Action Items
0-6 Months
< tr />
< td >6-12 Months
< td Begin infrastructure enhancements initiate extensive training programs personnel
< tr />
< td >1-3 Years
< td Conduct comprehensive reviews integrate feedback adjust policies accordingly